As the coronavirus pandemic forced the nation into lockdown in March 2020, patients were still able to have remote medical consultations with their specialist or GP from the safety of their own home. This has been possible thanks to the way in which telemedicine is changing healthcare.

Telemedicine encompasses the diagnosis and treatment of patients remotely using telecommunication technology, such as phone, video, and messaging services. The use of telemedicine wasn’t new in Australia prior to the COVID-19 crisis but it has been operating on a much larger scale over the last year, particularly in rural areas.
Capterra surveyed more than 1,000 Aussies who have had a doctor’s appointment within the last 12-months. We wanted to understand the benefits and challenges patients may have faced if they did experience remote healthcare and whether they will want to use it again in a post-pandemic world.
*To see a detailed methodology of the survey, skip to the bottom of this article.
92% of telemedicine users surveyed experienced it for the first time during the pandemic
Over half of Aussies surveyed were already familiar with telemedicine. Capterra’s survey discovered that 53% of respondents had used telemedicine before. It seems, however, that COVID-19 boosted the use of telemedicine with 92% of this group admitting that they used it for the first time during the crisis.
The increase in telemedicine usage may have been triggered by COVID-19 restrictions, but 84% of those who first experienced telemedicine during the pandemic said the reason behind their online consultation was unrelated to symptoms of the virus itself.
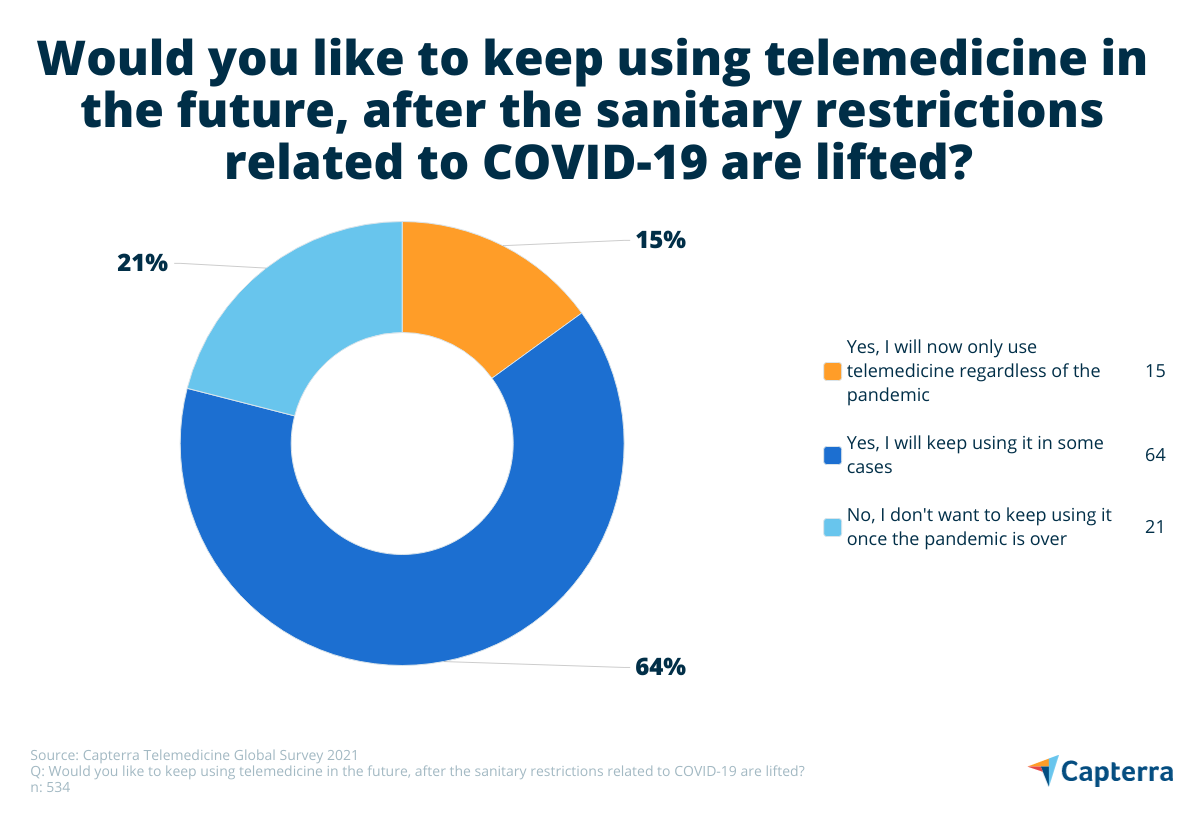
It seems for the most part that Australians are warming to telemedicine with a total of 79% of respondents saying they would use it again. This could be down to a range of reasons, including not needing to take time off work and not having to travel and pay for transport costs.
The benefits of using telemedicine
Throughout the pandemic, telemedicine may have been beneficial in keeping patients and doctors from catching or spreading COVID-19 during an in-person appointment.
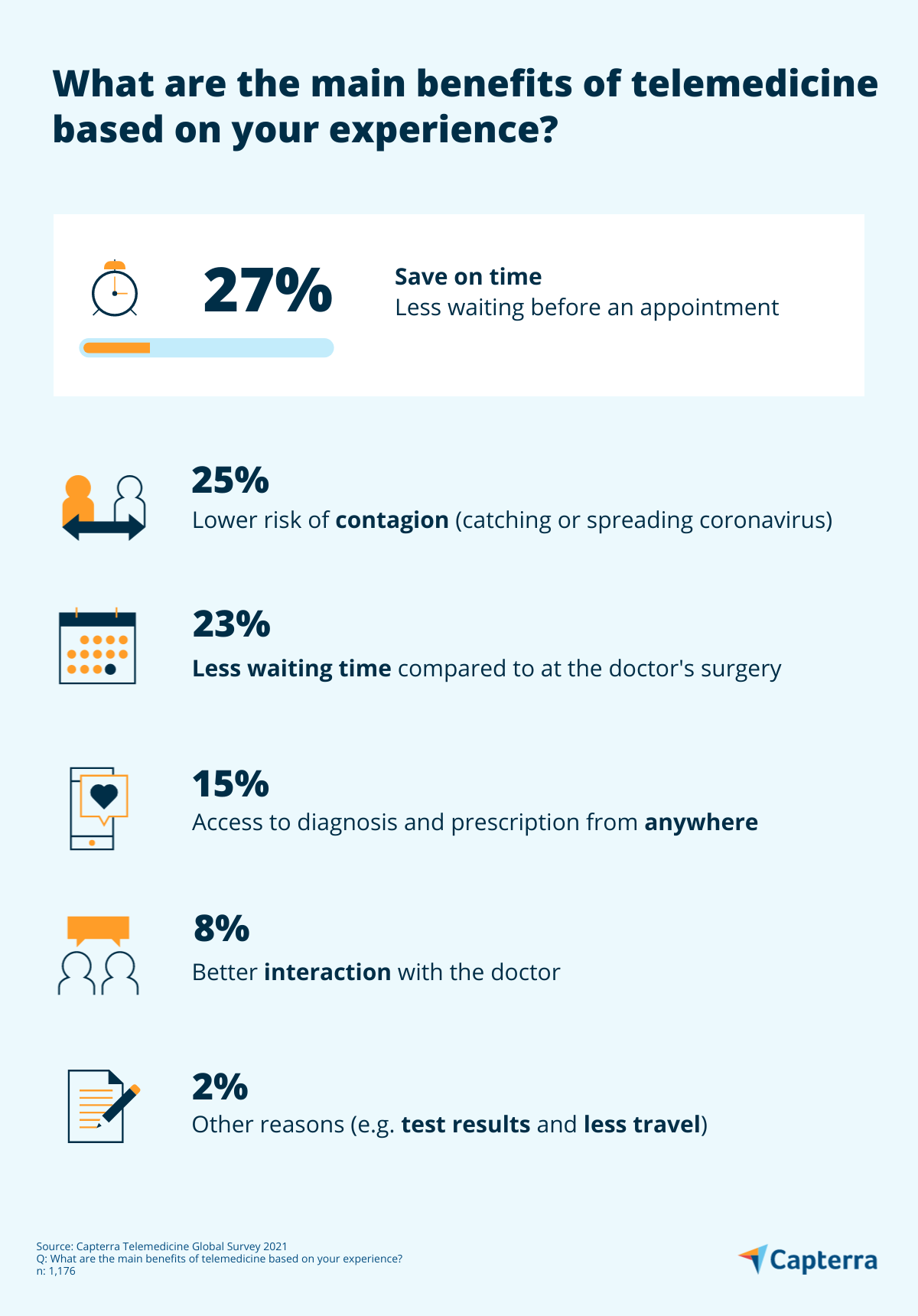
When we asked respondents what the main benefits of telemedicine were based on their experience, 27% answered that there was less waiting time before their appointment, and similarly 23% acknowledged that there was less waiting time overall compared to visiting the doctor’s surgery.
25% cited the risk of contagion being lower than physically going into a clinic as a reason for choosing telemedicine, and 15% found it beneficial that telemedicine enabled them to have access to a diagnosis and prescriptions from anywhere.
Other benefits of telehealth services as mentioned by respondents included:
- Follow-up appointment after treatment.
- Online sessions with their psychologist/ psychiatrist.
- Receiving test results (such as blood tests or X-rays).
- Having a consultation with a doctor who lives in another state.
- Saving time on distance and travel.
72% of users said that a teleconsultation was enough to solve their problem
Survey results show that almost half of respondents that used telehealth services did so for an online appointment with their GP (43%). Other popular specialties included psychiatry (7%), allergy and immunology (5%), and radiology, paediatrics and cardiology, which tallied 4% each.
Within the group of respondents who answered that they had used telemedicine for the first time during the COVID-19 pandemic, the large majority (72%) said that their medical problem was solved via teleconsultation. 11% of patients needed another online consultation with the same doctor, however, 12% needed an in-person appointment for their medical problem.
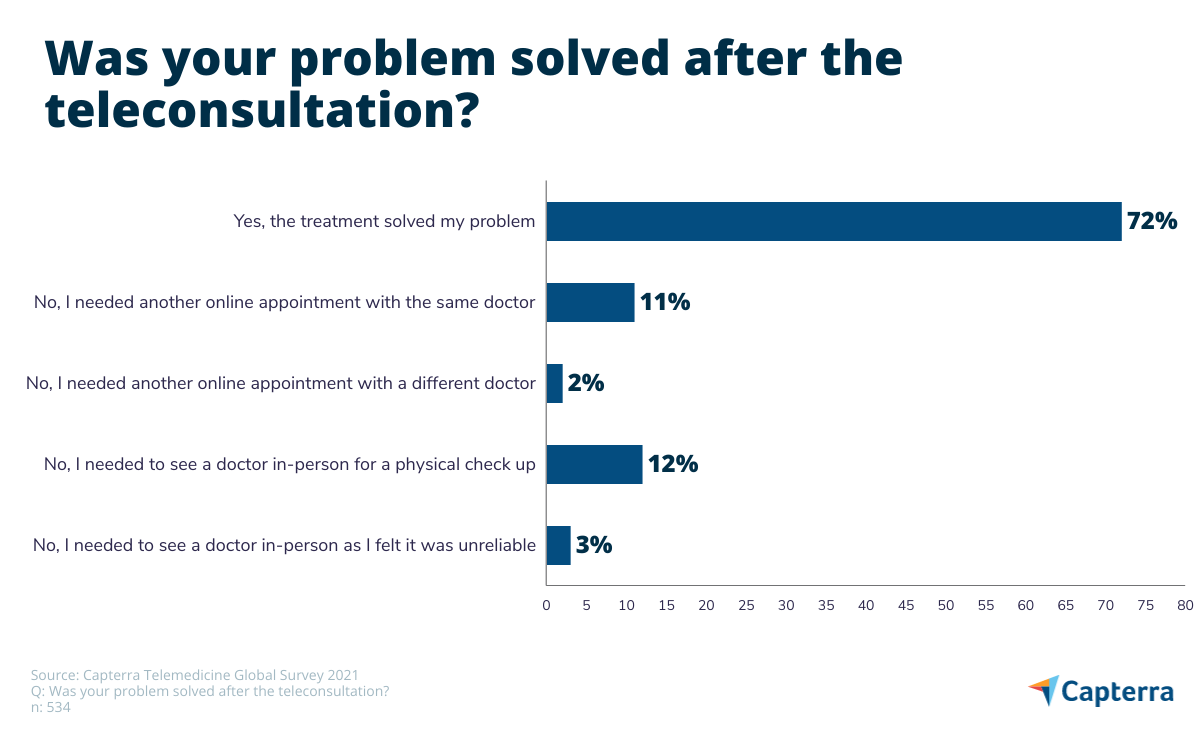
A small minority (3%) felt that the online consultation was not reliable enough and they needed to see their doctor at their practice. 2% needed another online appointment with a different doctor.
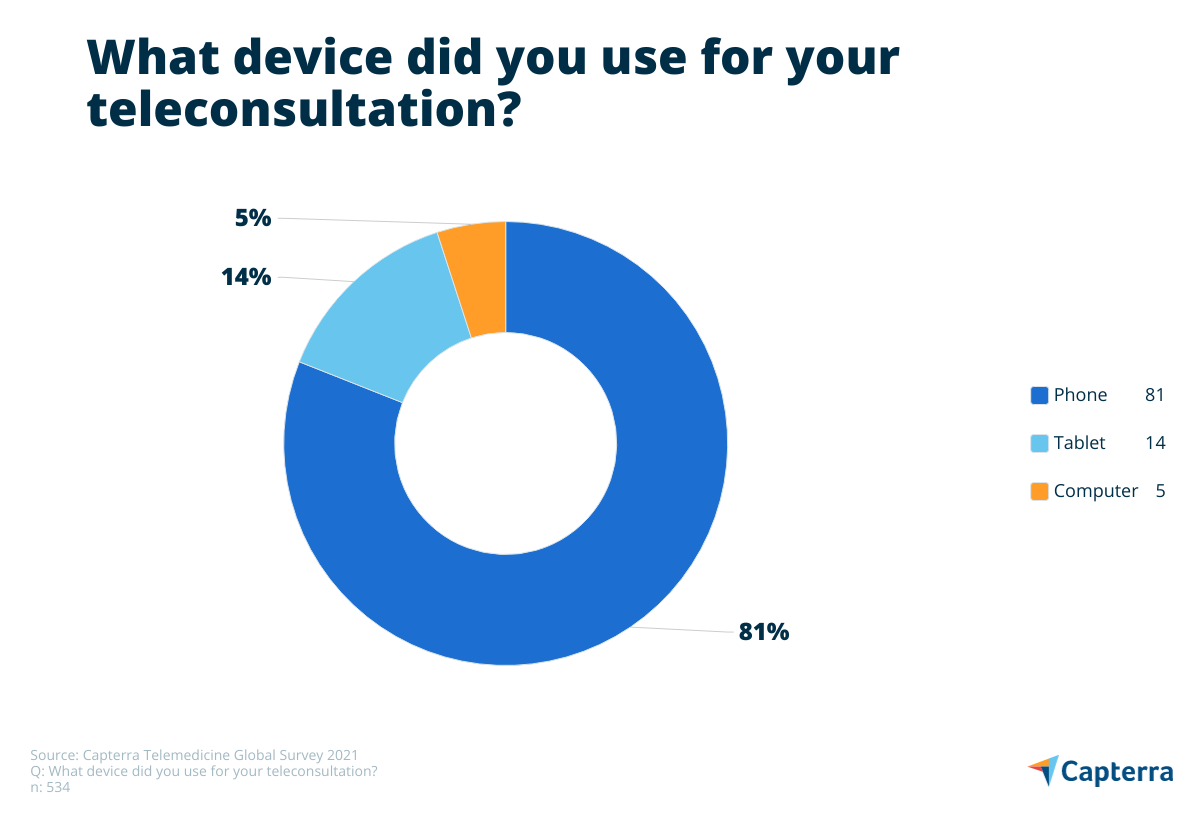
Telecommunication via phone call was most popular
There are many different ways to deliver telemedicine and each practice may have different options and services for their patients to use. We asked respondents which method they used when having a teleconsultation.
- 79% of respondents spoke to their doctor via phone call.
- 13% used a medical video conference app.
- 6% used an app or platform provided by their health insurance or doctor’s practice.
- 2% communicated via a messenger service, such as WhatsApp.
- Less than 1% selected “other,” using Zoom or FaceTime, for example.
Mobile phones were the most popular device utilised when it came to using telemedicine services, which could be down to the fact that they can be used for both phone calls and video conferences.
More than 1 in 5 won’t continue using telemedicine after the pandemic
Not everyone was pleased with remote healthcare, however, as the Capterra study found that 21% of participants who had already used telemedicine said they would not use it in the future. 47% of these respondents answered that they would feel more comfortable in person, and 41% would require a physical examination.
Other reasons for not using telehealth services included possible technical glitches and the lack of trust in data privacy (both 2%).
The challenges of telemedicine
Despite the many benefits associated with telemedicine, only 8% of respondents felt that they had a better interaction with their doctor remotely as opposed to in person. Whilst telemedicine may be useful for patients because of its on-demand options, it does come with a few challenges.
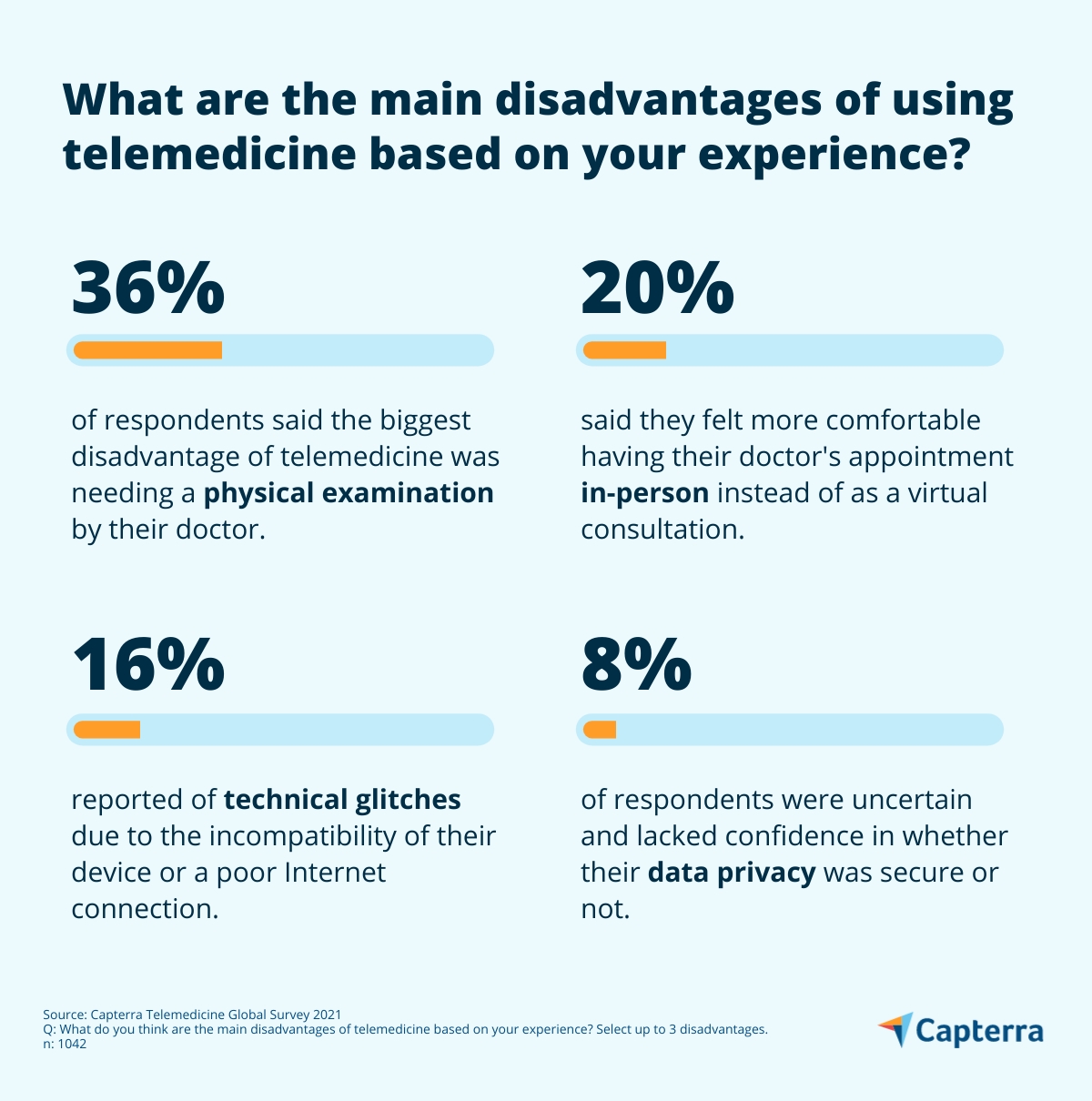
According to our survey, 36% of respondents found that one of the main problems with telemedicine was not being able to receive a physical examination. Some assessments may be difficult to make as the doctor cannot physically touch or feel the patient. 20% of respondents said that they would feel more comfortable seeing their doctor in person.
16% reported technical problems on either their side or on the doctor’s due to the device or a poor Internet connection. Some respondents answered that they did not know whether their personal data was secure enough (8%), and others stated that they lacked privacy in their own home, which may be due to living in a shared household (7%).
7% of patients noted that the “unpreparedness of their health professional” was a challenge. This may be because of resistance from some physicians in the use of new technology.
How might telemedicine software offer a solution?
In order to discover what it would take for patients to continue using telemedicine, we can look at the challenges that our respondents faced and see how telemedicine technology can help.
Telemedicine software generally offers features to make the end-to-end process easier, such as scheduling tools that enable patients to see the doctor’s calendar in real-time and book an online appointment. Healthcare professionals may also have access to the patient’s electronic health record (EHR) to check their medical history before a consultation and also add new information to it afterward. A chatbot may prompt a patient to answer questions about their symptoms and suggest the next steps that they should take, such as booking a consultation.
Physicians can still administer a physical examination using video technology as patients can follow guided instructions from their doctor. Using a video conferencing app in real-time, the doctor can talk the patient through self-examination and ask them to make certain maneuvers. For example, they can show the patient how to check their tonsils for any lumps, to check their own pulse, and to perform breathing techniques to check for wheezing or coughing.
Australia has strict patient privacy and confidentiality laws that also apply to telehealth services. Medical professionals need to choose a platform that is HIPPA compliant and bound by the Privacy Act 1998. Patients must be advised on how their personal details will be collected and stored and give consent before engaging in a telemedicine service. These privacy laws should give reassurance to patients who lack confidence in the security of their personal data.
Capterra’s survey results highlight that there has been an increase in the use of telemedicine software since the start of the pandemic and it could be argued that the benefits of using remote healthcare outweigh the challenges. With patients having access to healthcare advice regardless of their location or situation, it makes sense that respondents will continue to use these convenient services in the future. In the next article in this two-part series, Capterra explores how patients feel about the use of AI in healthcare, including whether they have any data privacy concerns.
*Survey methodology
To collect the data for this report, we conducted an online survey in April 2021. Of the total respondents, we were able to identify 1,008 Australians who adhered to the following criteria:
- Resident of Australia
- Over 18 years of age
- Had a healthcare appointment within the last 12 months
- Visits the doctor at least once a year.
